
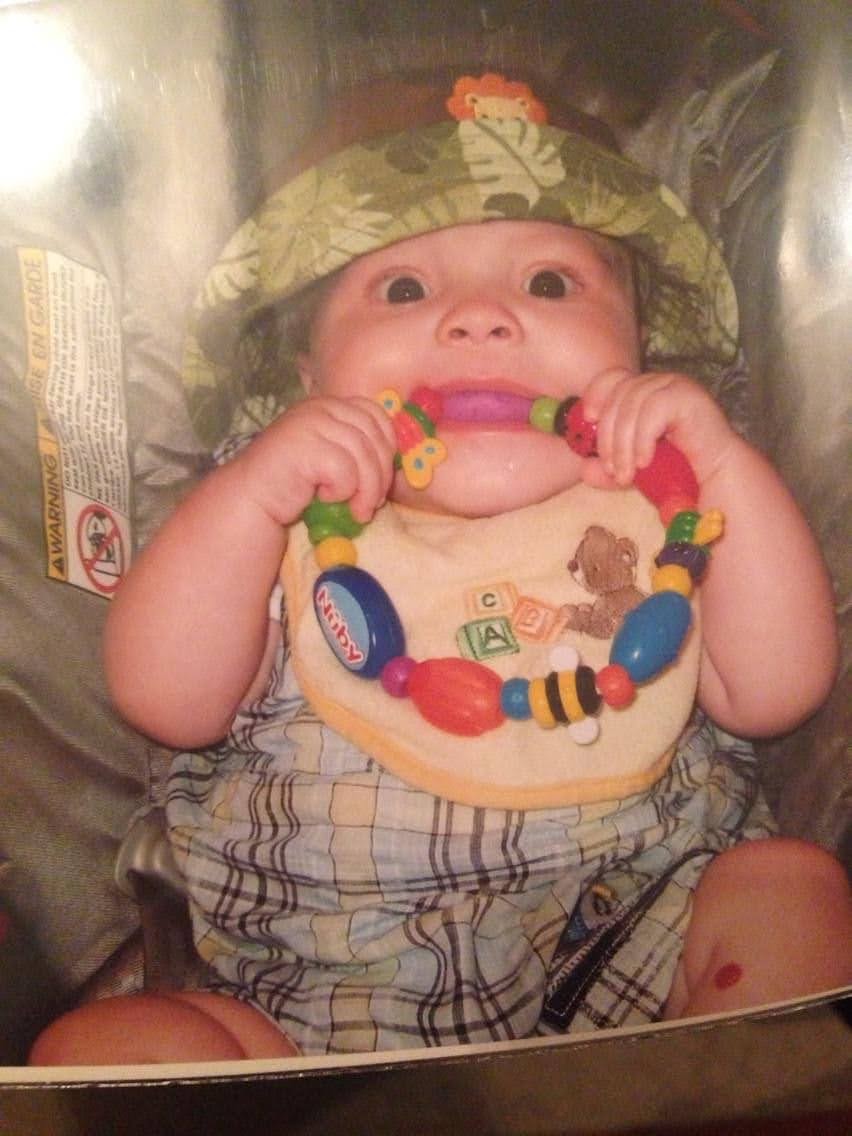
By definition, rare implies both uncommon and unusual. Luca was rare. A treasure. When I look back, even from the beginning of his life, there were signs pointing to how my little man, the one who made me a mom, would be exceptional.
There is a 5-12% chance that a neonate will pass meconium within the amniotic fluid after 37 weeks’ gestation. A small proportion of this select group of neonates will swallow meconium and require intervention to assist with breathing. Luca was one of those neonates who swallowed meconium, however he did quite well and required only minor assistance at delivery.
Once delivered, he was quickly whisked away also because he was born with a condition called hypospadias. A birth defect that affects 1 in every 250 males (less than 0.5%). This is a common birth defect where the urethra (pee hole) is not on the tip of the penis, but rather on the shaft. Anatomically, everything works as it should, but the location of the urethra needs adjusting. He was also born with a tiny round hemangioma on this leg. Less than 10% of infants develop a benign hemangioma, and those that do are usually pre-term and weight very little. Luca was a full-term normal weight infant.
I remember we were told by his pediatrician that the urology team at our local hospital would never consider doing surgery on an infant his age to correct hypospadias, he was too young. So, his pediatrician shared with us that he wasn’t even going to send in a referral to urology until he was over a year old. So, we had to wait. I was looking forward to that “mom milestone” when your baby boy ‘tinkles’ on you during a routine diaper change. Everyone talked about it happening. Friends and family even purchased ‘pee-pee teepees’ for my baby shower in anticipation of this. It never happened. Once, when changing Luca’s diaper, the sun was shining through the window. I saw a spider web. I tried brushing it away only to realize that was not what it was. It was Luca’s pee! The stream was so thin. When he was finally referred for surgery the urologist scolded us for not bringing him in sooner. He said we would now run the risk of causing him anxiety and that they prefer to do the surgery when they are younger, if possible. This was our first taste of how ‘experts’ in the medical system give advice on areas they really know very little about. And they get away with it.
Following his surgery, we were told Luca would do very well. He was quoted a low 1-5% overall risk to develop a complication, specifically a fistula, from the surgery within the first year. We heard his urology team talk about how these complications are rare, they do this surgery routinely. Several years later, Luca became very agitated in the washroom and called out for me “Mommy mommy mommy, come quick, my pee is coming out of two different holes!!! Mommy hurry help!!”. You could hear the fear in his voice. My heart sank, adrenaline started pumping as I ran towards him. This was just one of the many moments I had while Luca was alive where I had to mask my fear, put on a brave face, and reassure Luca things will be okay.
Luca had developed a fistula.
Luca had developed a fistula almost four years following his hypospadias repair that required a second surgery to repair. His urologist told us he has never seen that before. Since his fistula was not life-threatening, he had to wait several months for surgery. Imagine being in kindergarten having to go to the washroom around other children and being too young to explain to others why your pee is coming out of two openings. It was a lot for him to deal with at that age. His urologist told us he was just about to discharge Luca and assumed his fistula happened because he must have been holding in his pee too long during the day sometimes. It took a while for Luca to brush that off. He was angry at himself and then was terrified if he had to pee and couldn’t get to a washroom within 30 seconds. This was problematic in the car and led to a lot of anxious meltdowns and stressful situations in the car. It is too bad specialists can’t find a way to talk to parents without the children in the room.
The repair surgery caused him a lot of post-traumatic stress just as the urology team had warned us it would. Luckily children are resilient and after a few months he was alright. One of the traumas forever in our mind was the night before we had to return to the hospital to have his catheter removed. His penis was wrapped tight in bandages to hold the catheter in place. We were told to just simply put him in the bathtub one or two nights before his apt, and the material would just ‘fall off’. The first night, after two hours soaking in the tub, it did not fall off. It would not even come off the tiniest bit if we tried pulling it off. The second night, Luca spent more than an hour soaking and still, the bandage would not come off. We had one corner slightly peeled off but every time we approached Luca he would violently kick and scream while sobbing. He was scared removing the bandage would hurt. We had never seen him like this, he was so protective of his body and angry whenever we tried to remove the bandage. One of us had to hold him down while the other tried to remove the bandage. We took turns but nothing was helping. It was not coming off. We were all in tears out of sheer frustration.
As a last resort, because it was getting very late, we called the afterhours on-call urologist. The helpful advice we were given was ‘Well, I don’t know what to say it should come right off in the water after soaking. It needs to come off our we can’t take the catheter out and then you will have to make another appointment’. No other options or even encouragement was provided while we suffered through this. I finally took to Facebook and posted a plea and a friend who is a physician told us to try rubbing baby oil on it. Worked instantly.
In Luca’s early years he had a few interesting symptoms. I remember a few times in the early spring he would run around the backyard and he’d come in with blue lips. He was around 2.5 years old. When we requested an appointment with his pediatrician to discuss this, it was dismissed right away as being normal. I was worried Luca had a heart condition. We were told if it keeps happening we will worry about it. Fortunately, it stopped happening. I wondered if maybe he was just sensitive to the cold temperature. I have Raynaud’s disease. I was diagnosed when I was 12 years old. Perhaps this was something he had too? He also had a small lump the size of a pea on the side of his neck when he was an infant that his pediatrician said was a swollen lymph node. I wondered if maybe be had mononucleosis? I had mono once when I was 15. I didn’t have the typical symptoms I just had a lump on the side of my neck I found unexpectedly while putting my hair up into a ponytail. My wrist brushed the side of my neck and to be honest I thought I had a bad reaction to a bug bite. I was 15 years old. I was a bit more tired than usual, however within a month it resolved. I was fine. I worried something was wrong with Luca because his ‘swollen lymph node’ remained for longer than six months. I don’t remember my ‘mono lymph node lump’ lasting so long. Many relatives on my husband’s side have cancer, so then I started to worry Luca had cancer. It seemed like my worrying was unjustified and there wasn’t any concern about these things I worried about or asked his pediatrician about.
Luca also had some dental issues. He had enamel hypoplasia that his specialized dentist indicated he was likely born with. He had to use a special toothpaste and he was prone to cavities. We always brushed his teeth and gums when he was a newborn, and never let him go to sleep after a bottle. I don’t know why this happened to him. Enamel hypoplasia isn’t common among children, approximately only 8-10% of children experience this.
When Luca was diagnosed with ITP at age 7 we were shocked.
When Luca was diagnosed with ITP at age 7 we were shocked. How did he develop this? The incidence of ITP in children is estimated in literature to be approximately 1.9 to 6.4 cases per 100,000 per year. And of that select group, only 20% have the chronic lifelong form of the disorder as a child. Only 3-4% of children with ITP will experience serious bleeding such as prolonged nose bleeds, hematuria (blood in urine), gastrointestinal bleeds, stomach bleeds, ocular bleeds, oral bleeds and blood blisters. And an even smaller amount will be refractory to steroids and IVIG. Luca had all of these things. Including a brain bleed that wasn’t addressed in a timely fashion that he ultimately died from. He also used to get what looked like petechia on his front incisors, but his hematologist said it was not related to ITP. We never did learn what it was.
As a trained genetic counsellor, I was always trying to connect his symptoms. Maybe he had a genetic syndrome. But nothing fit, and one of the geneticists I worked with didn’t think there was any connection between Luca’s physical traits (hemangioma, hypospadias) with severe thrombocytopenia. There is a hereditary hemangioma-thrombocytopenia syndrome, but Luca only had the one tiny benign hemangioma. It was the size of a pencil eraser. At the time, there was only one genetic testing company I could find offering panel testing for thrombocytopenia months before he died, but Luca did not fit into the criteria at that time. We did not have a family history of thrombocytopenia, and he did not have an enlarged spleen or an enlarged liver. It’s still in my thoughts that perhaps there is a unifying reason for all these things.
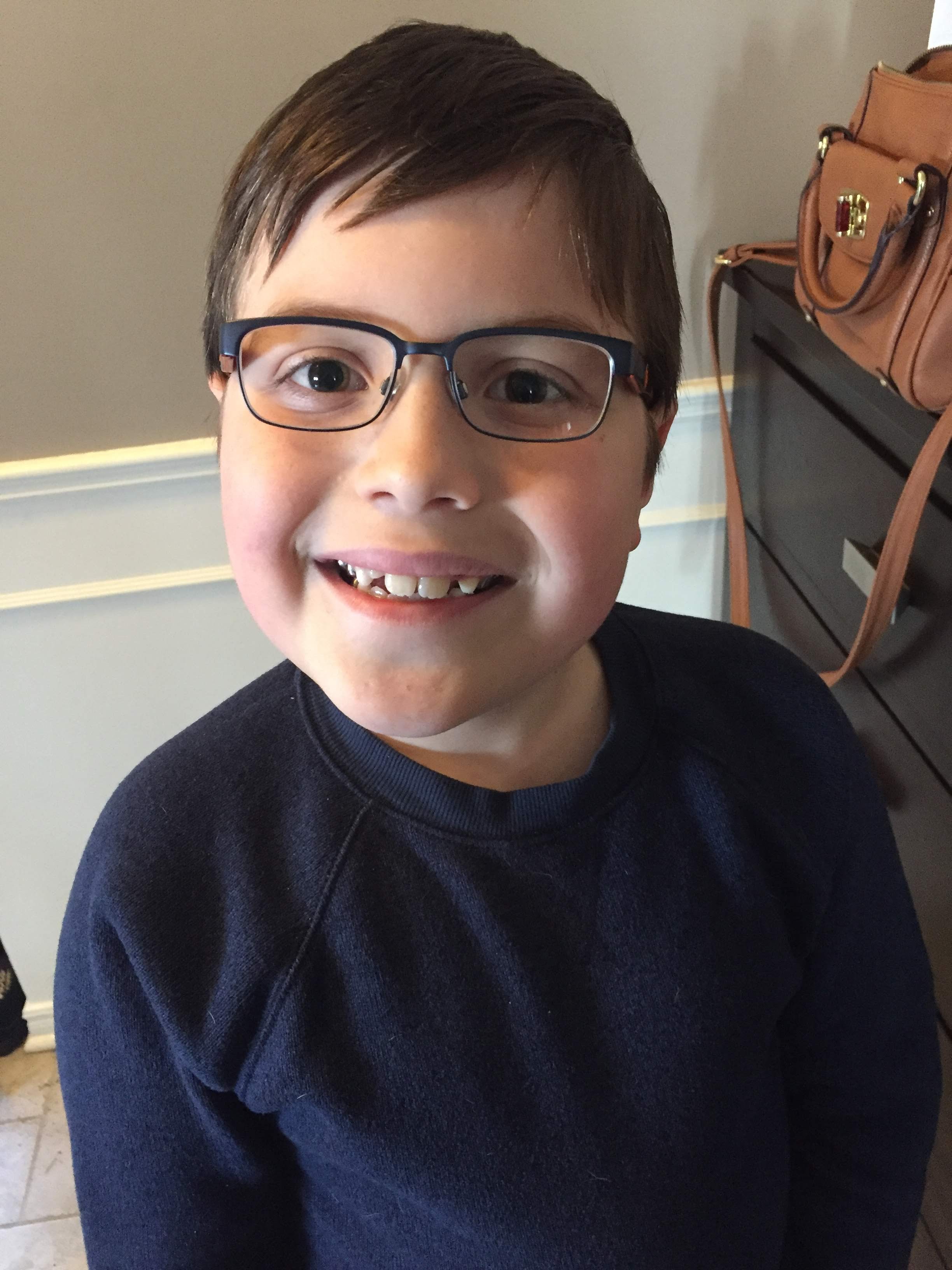
At the start of third grade, Luca complained about his eyesight. We took him in to see his pediatrician and after testing his eyesight, he said he was just fine. A few months later he was still experiencing difficulties seeing during class, so we took him to Lens Crafters at Costco, and the optometrist was shocked by how he was managing with such poor eyesight. We immediately got him glasses, two pairs in case one broke or he lost one and shook our heads that once again his pediatrician provided us with ‘garbage’ information. While both my husband and I wear glasses, neither of us required glasses as a child. In fact, neither of us could even think of anyone in our family who required glasses as a child.
About six weeks or so before Luca passed away, we had taken him to Lens Crafters again to get his eyes re-tested. He had started to complain once again that he was not seeing well at school. We had mentioned his previous steroid use, so they tested his ocular pressure, and in both eyes the pressure was elevated. This is rare for a child. The plan was to repeat this assessment in three months, and if there was no change he would be referred to another specialist for early glaucoma prevention. Unfortunately, he passed away before we he could have this reassessed. I remember posting on the Platelet Disorder Support Association (PDSA) Facebook page to see if anyone with ITP, particularly those that used steroids, developed glaucoma. It was not a side effect we were ever told about, and what I could look into myself using the internet seemed to imply the risk was for long term steroid use – not a few short pulse treatments.
When Luca had his brain bleed, he did not present the traditional way in which we were counseled to watch for. He did not have a progressive thunderclap headache that was unresponsive to Tylenol and got worse over time. In fact, this headache was not even as bad as when he had suspected aseptic meningitis following IVIG the first time he used it. Aseptic meningitis as a reaction is not typical (0.5-11%), but well documented in a significant number of individuals with ITP. His headache due to the brain bleed resolved with Tylenol but returned within a 12-hour period. He presented more with lethargy and symptoms his specialist team were confident were due to ‘a bug’. The overall risk to develop a brain bleed as a child with ITP is less than 1%
Most brain bleeds with ITP are more of the subdural hematoma type. Luca developed a left lobar hematoma with a small subarachnoid component, and due to the increased prolonged intracranial pressure there were multiple infarcts noted with some bleeding deeper in his brain. So once again, he is not presenting in the same way. Following his first craniectomy he required another one because the intracerebral pressure was too great. This also isn’t typical. It also wasn’t typical that before his first craniectomy, Luca’s pupil become ‘unfixed’ and there was hope he would make it, but that didn’t happen. More than 50% of individuals with ITP who have a brain bleed survive with often non-serious neurological sequalae, if detected early.
When I hear the phrase “it’s not expected” or “it’s not likely” or “it’s very rare” I just roll my eyes. Calling something rare is completely subjective. For instance, 1% is still one in every 100 people. So really that isn’t really a rare risk. When you are dealing with rare things, over-confidence can be destructive.
Depending on how you define what a rare disease is, approximately 1 in 12 people on this planet have a rare disease. Yet, physicians in medical school are still learning to look for horses instead of zebras when they hear hoof steps. And worse, specialists become so obtuse about things they see. They fail to reach out to other specialists when the usual becomes atypical. Luca deserved better. I believe he should still be here with us.